Thyroid disorders serve as an umbrella term for conditions that disrupt the normal functionality of the thyroid gland. These disorders impact over 200 million people worldwide and more than 20 million in the United States as of 2025. Shockingly, research shows that over 60% of those affected remain unaware of their condition, silently enduring symptoms that could be managed with proper care. This blog will talk in detail about thyroid disorders, unpacking everything from early warning signs to cutting-edge treatments, so you can take control of your health.
Table of Contents
- What is the Thyroid Gland?
- Symptoms of Thyroid Disorders
- Types of Thyroid Disorders
- Risk Factors for Thyroid Disorders
- When to See Your Doctor
- Thyroid Treatments and Medication
- A Word from Doctor Zara
- Frequently Asked Questions
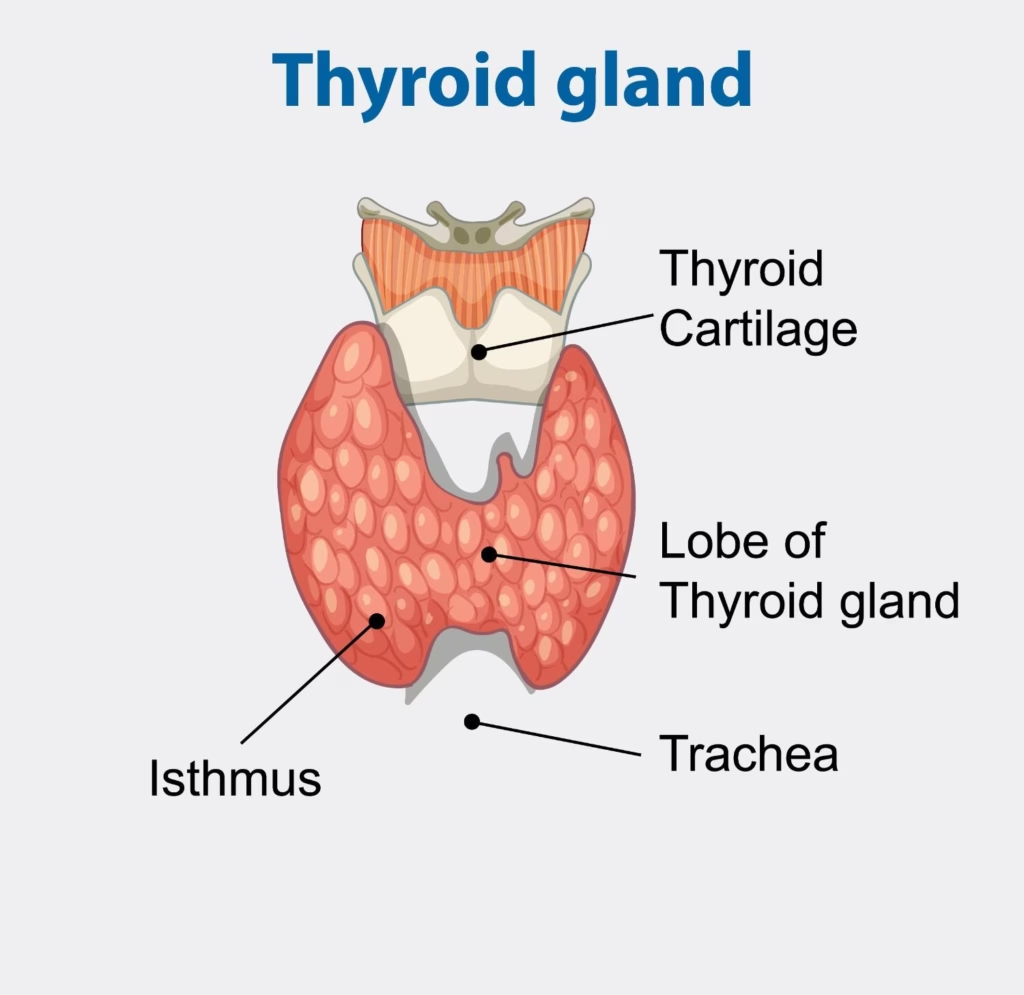
What is the Thyroid Gland?
The thyroid gland is a butterfly-shaped endocrine gland located at the front of your neck, just below the Adam’s apple and under your skin.
As part of the endocrine system, it plays an important role in regulating body functions by producing and releasing hormones.
These hormones influence everything from your heartbeat to how efficiently your body burns calories.
Functions of the Thyroid Gland
The thyroid gland’s hormones are like the conductors of your body’s symphony, ensuring every system runs smoothly.
Here are the key functions of the hormones it produces:
- Regulate Metabolism: Triiodothyronine (T3) and thyroxine (T4) control the speed of metabolism, converting food into energy for cellular activities.
- Support Cardiovascular Health: T3 and T4 influence heart rate and blood pressure, ensuring efficient circulation and oxygen delivery.
- Maintain Body Temperature: These hormones help regulate body heat by adjusting energy production and expenditure.
- Promote Growth and Development: T3 and T4 are critical for brain development in infants and physical growth in children.
- Regulate Calcium Levels: Calcitonin lowers blood calcium by promoting its storage in bones, supporting bone health and preventing osteoporosis.
- Influence Digestion and Muscle Function: Thyroid hormones ensure proper digestion and muscle strength by modulating energy availability.
Symptoms of Thyroid Disorders
Thyroid problems often sneak up subtly, but recognizing the signs early can make all the difference. There are numerous symptoms associated with thyroid disorders, and we’ve compiled 19 common ones to help you identify potential issues. Here is the list of the most common symptoms of thyroid gland disorders;
General Symptoms
- Slow or rapid heart rate
- Muscle and joint pain
- Unexplained weight loss or gain
- Sensitivity to heat or cold
- Depression and anxiety
- Fatigue and weakness
Thyroid Symptoms in Women
Thyroid symptoms in females often tie into hormonal fluctuations, making them especially disruptive.
- Irregular menstrual cycles
- Hair thinning or loss
- Changes in skin texture
- Puffy face
- Constipation or diarrhea
Thyroid Symptoms in Men
Men might notice less obvious shifts, but these can still impact daily life significantly.
- Mood changes
- Reduced sex drive
- Hoarse voice
Often Overlooked Symptoms
These sneaky signs are frequently dismissed as stress or aging, but they could signal thyroid imbalance.
- Dizziness and balance issues
- Dry or itchy skin
- Brain fog (forgetfulness)
- Enlarged neck (goiter)
- Brittle nails
Types of Thyroid Disorders
As mentioned, thyroid disorders encompass various conditions affecting the gland’s function. The most common include:
- Graves’ disease
- Hashimoto’s thyroiditis
- Thyroid nodule
- Thyroid cancer
- Hypothyroidism
- Hyperthyroidism
- Thyroiditis
- Goiter
Let’s break them down for clarity.
Graves’ Disease:
This is an autoimmune disorder that causes the thyroid to overproduce hormones, leading to hyperthyroidism. It often results in symptoms like rapid heartbeat and weight loss, and can lead to thyroid eye disease, where eyes bulge or become irritated. The ICD-10 code for Graves’ disease with thyroid eye disease is typically E05.00.
Causes:
- Autoimmune factors
- Genetics
- Stress
Hashimoto’s Thyroiditis:
This is an autoimmune condition where the immune system attacks the thyroid, gradually leading to hypothyroidism. It progresses slowly, causing fatigue and weight gain as hormone production dwindles.
Causes:
- Genetic predisposition
- Environmental triggers
- Viral infections
Thyroid Nodule:
These are lumps in the thyroid, often benign but sometimes requiring evaluation for cancer. Thyroid nodule ICD-10 is E04.1 for nontoxic single nodules. Lingual thyroid, a rare ectopic nodule in the tongue, falls under E07.89.
Causes:
- Iodine deficiency
- Inflammation
- Overgrowth of normal tissue
Types:
- Solid
- Cystic
- Mixed
Thyroid Cancer:
A malignancy starting in thyroid cells, often treatable if caught early. It may present as a nodule or enlarged gland, with rising cases globally in 2025.
Causes:
- Radiation exposure
- Genetic mutations
- Family history
Types:
- Papillary
- Follicular
- Medullary
- Anaplastic
Hypothyroidism:
This occurs when the thyroid underproduces hormones, slowing metabolism. Common causes include Hashimoto’s, leading to symptoms like fatigue and cold sensitivity. Thyroid disorder ICD-10 for unspecified hypothyroidism is E03.9.
Causes:
- Autoimmune disease
- Iodine deficiency
- Medications
Hyperthyroidism:
The opposite of hypothyroidism, where excess hormones speed up bodily functions. It can cause anxiety, heat intolerance, and weight loss.
Causes:
- Graves’ disease
- Toxic nodules
- Excessive iodine
Thyroiditis:
Inflammation of the thyroid, which can be acute or chronic, temporarily disrupting hormone levels.
Causes:
- Viral or bacterial infection
- Autoimmune response
- Drug reactions
Types:
- Acute
- Subacute
- Chronic
Goiter:
An enlarged thyroid gland, visible as neck swelling, often due to iodine issues but not always impairing function. It can be diffuse or nodular.
Causes:
- Iodine deficiency
- Hormonal imbalances
- Inflammation
Risk Factors for Thyroid Disorders
The risk factors for thyroid disorders are closely tied to their causes, but understanding them can help you mitigate potential issues. Three main categories stand out: genetics, lifestyle, and autoimmune factors. Let’s explore how these play into your thyroid health.
Genetics
Genetics form a foundational risk, as family history significantly increases your chances of developing thyroid issues. If a parent or sibling has Hashimoto’s or Graves’, you’re more likely to inherit susceptibility genes that affect immune regulation or hormone production. Studies have identified shared genetic markers between autoimmune thyroid diseases and other conditions, highlighting a strong hereditary link. While you can’t change your DNA, awareness prompts earlier screening.
Lifestyle
Lifestyle factors play a critical role in thyroid health, acting either as protective or provoking influences. Poor diet, particularly inadequate iodine intake, disrupts hormone synthesis, while excessive iodine from supplements can trigger hyperthyroidism. Smoking intensifies autoimmune responses, and chronic stress weakens immune tolerance, fostering inflammation. Radiation exposure from medical treatments or the environment increases thyroid cancer risk, while sedentary behavior and obesity impair thyroid function over time.
Protective strategies include:
- Maintaining balanced iodine intake through foods such as seafood and dairy
- Engaging in regular physical activity
- Practicing stress-reduction techniques like meditation or yoga
- Avoiding exposure to environmental toxins
Auto-immune
Autoimmune factors are central to many thyroid disorders, where the body’s immune system mistakenly attacks the gland. Conditions like Hashimoto’s arise from this self-sabotage, often triggered by environmental factors interacting with genetic vulnerabilities. Women are at higher risk due to hormonal influences, and infections or gut microbiome imbalances may initiate the process. Early detection through antibody tests can help manage progression.
When to See Your Doctor
Don’t wait for symptoms to overwhelm you, early intervention is key to managing thyroid disorders effectively. If you notice any of the signs of thyroid problems outlined above, especially persistent fatigue, weight changes, or neck swelling, schedule a visit promptly. Your doctor will conduct a physical exam and may order tests to confirm a diagnosis, helping rule out or address issues like hypothyroidism or hyperthyroidism.
Possible tests and examinations include:
- Blood tests for TSH, T3, T4, and thyroid antibodies
- Ultrasound of the thyroid
- Radioactive iodine uptake scan
- Fine-needle aspiration biopsy for nodules
- Neck palpation during physical exam
Thyroid Treatments and Medications
Treating thyroid disorders isn’t one-size-fits-all, but options range from simple medications to advanced procedures, ensuring most cases are manageable. These can restore hormone balance, shrink enlargements, or eliminate cancerous cells. The three main approaches are medications, surgery, and chemotherapy/radiotherapy. They offer tailored paths to recovery, often combined for optimal results.
Medications
Medications form the frontline treatment for many thyroid issues, aiming to normalize hormone levels without invasive steps. For hypothyroidism, synthetic hormones replace what’s missing, while hyperthyroidism drugs block excess production. Regular monitoring ensures dosages stay effective, and side effects are minimal with proper use. Beta-blockers may be added for symptom relief like heart palpitations.
- Levothyroxine: A synthetic T4 for hypothyroidism, taken daily to boost metabolism; it’s safe long-term with blood test adjustments.
- Antithyroid drugs (e.g., methimazole): Reduce hormone production in hyperthyroidism; effective for Graves’ but may require months to years.
- Beta-blockers (e.g., propranolol): Control symptoms like tremors or rapid heartbeat without altering hormone levels directly.
Surgery
Surgery becomes necessary when medications fail or for issues like large goiters or cancer, removing part or all of the thyroid to resolve the problem. Advances in minimally invasive techniques reduce recovery time and risks like voice changes. Post-surgery, hormone replacement is often needed to maintain balance.
- Partial thyroidectomy: Removes one lobe, ideal for single nodules; preserves some natural function.
- Total thyroidectomy: Removes the entire gland, common for cancer or severe hyperthyroidism; followed by lifelong medication.
- Lymph node dissection: Added if cancer has spread, to prevent recurrence.
Chemotherapy and Radiotherapy
These targeted therapies are reserved for aggressive cases, like advanced thyroid cancer, using drugs or radiation to destroy malignant cells. Radiotherapy, especially radioactive iodine, is highly effective as thyroid cells absorb it selectively. Chemotherapy complements when cancer resists other treatments, though side effects like nausea require management.
- Radioactive iodine therapy: Oral dose that targets thyroid tissue; used post-surgery for remnants or hyperthyroidism.
- External beam radiation: Focused beams for inoperable tumors; precise to minimize damage to nearby areas.
- Chemotherapy drugs (e.g., doxorubicin): Systemic for metastatic cancer; combined with others for better outcomes.
A Word from Doctor Zara
Thyroid disorders impact millions globally, yet many dismiss early signs as mere fatigue or stress, don’t make that mistake. Taking symptoms seriously can lead to timely diagnosis and life-changing treatment, preventing complications down the line. If you’re experiencing any red flags, consult a healthcare professional immediately for personalized guidance. For questions or to connect with a qualified expert, feel free to email me at drzaramulla@gmail.com. Remember, this advice isn’t a replacement for professional medical checkups or appointments, prioritize your health with regular visits.
Frequently Asked Questions
Q: What are the early warning signs of thyroid problems in females?
Answer: Early signs often include fatigue, weight gain, irregular periods, and hair loss, which can mimic hormonal changes but warrant a check if persistent.
Q: What causes thyroid problems?
Answer: Causes range from autoimmune attacks and iodine imbalances to genetics and environmental factors like radiation.
Q: What is hypothyroidism?
Answer: Hypothyroidism is an underactive thyroid that doesn’t produce enough hormones, leading to slowed metabolism and symptoms like cold sensitivity.
Q: What is thyroid eye disease?
Answer: It’s an autoimmune condition linked to Graves’ disease, causing eye bulging, dryness, and vision issues; ICD-10 often pairs with E05.00.
Q: What is a lingual thyroid?
Answer: A rare congenital condition where thyroid tissue develops in the tongue base instead of the neck; ICD-10 is E07.89.
Q: What is the thyroid disorder HESI case?
Answer: This refers to case studies in nursing education (like HESI exams) simulating thyroid scenarios for training, often covering symptoms and management of disorders like hypothyroidism.

